In addition to onychomycosis, there are several other causes and diseases that can cause the normal appearance of nails to change.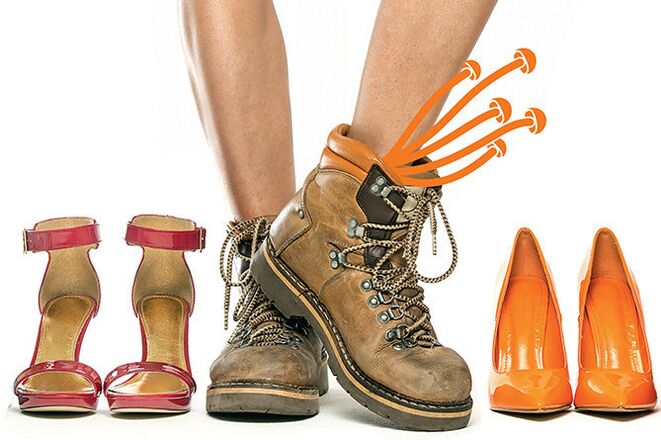 Thick, cloudy white nails can be the result of psoriasis or the failure of rough cosmetics. Detachment and detachment of the nail plate is associated with injuries and trophic disorders of the lower extremities in varicose veins or endocrine diseases. Onichomycosis very often does not begin with a change in the nail plate itself, but with redness, itching, and peeling of the skin surrounding the nail. If a person does not pay attention to these symptoms, the fungus begins to develop, penetrating deeper tissues, including. under the nail bed. Damage to the nail plate fungus usually begins at the free edge, which thickens, turns grayish-yellow, easily tears, and collapses. But even in this case, only laboratory research - microscopy can be used to accurately determine the presence of the fungus.
Thick, cloudy white nails can be the result of psoriasis or the failure of rough cosmetics. Detachment and detachment of the nail plate is associated with injuries and trophic disorders of the lower extremities in varicose veins or endocrine diseases. Onichomycosis very often does not begin with a change in the nail plate itself, but with redness, itching, and peeling of the skin surrounding the nail. If a person does not pay attention to these symptoms, the fungus begins to develop, penetrating deeper tissues, including. under the nail bed. Damage to the nail plate fungus usually begins at the free edge, which thickens, turns grayish-yellow, easily tears, and collapses. But even in this case, only laboratory research - microscopy can be used to accurately determine the presence of the fungus.
The fungus only appears in the elderly and in chronic patients.
In patients with chronic diseases (diabetes mellitus, peripheral vascular diseases, etc. ), nail fungus is indeed more common, but only because these diseases reduce the activity of general and local immunity, negatively affect the skin's resistance to any infection. Old age alone cannot be the cause of fungal diseases, but the older a person gets, the more health problems accumulate, which contributes to the development of fungal infections. However, completely healthy young people are not protected against onychomycosis. Sports lovers can suffer from nail fungus. calluses, microtraumas of the skin of the feet and sweating create ideal conditions for fungal development. Mushrooms can occur in those who have to spend most of the day on their feet, in closed shoes that do not allow excess moisture to evaporate. Smoking, frequent stress, and excessive love of sweets increase the risk of developing fungal infections.
The fungus is usually infected in a swimming pool, sauna or beach.
The risk of encountering the fungus in a sauna, pool, or on the beach is indeed very high than in any other place with high air temperature and humidity where the spores of onychomycosis pathogens remain viable for a long time. But this is by no means the only way to infect onychomycosis. The pathogens of fungal infections can get on the skin of a person visiting a gym, beauty salon, shoe store, public transport, or simply wearing other slippers. But contact with the fungus or its spores does not always lead to infection, much depends on the condition of the skin and the body as a whole. And only if the fungus is placed in the optimal developmental environment and finds a weak spot in the human body’s immune defenses can it damage the skin and nails. Risk factors for developing onychomycosis include dry skin hardening and cracking of the skin of the feet, increased sweating of the feet, tight and "non-breathable" shoes, and synthetic socks.
Fungal spores are found everywhere, there is no effective protection against them.
Fungal spores are indeed found almost everywhere, even at home, making it impossible to completely rule out contact with it. Yet, even those at high risk of developing mycosis have the opportunity to protect themselves from developing the infection. First, you must carefully follow the rules of personal hygiene: only your own shoes, towels, etc. It is just as important to carefully monitor the skin of your feet and nails - remove dry calluses in time, treat cracks, abrasions and cut your nails properly. It will not be unnecessary to prevent excessive foot sweating, including the use of antiperspirant products for the feet. If the risk of onychomycosis is very high, you can cover your nails prophylactically (once a week) with a special antifungal varnish. You can also start taking immune-boosting drugs - interferon inducers, herbal adaptogen-based drugs, multivitamin complexes - after consulting your doctor.
The mushroom is eternal. You can't get rid of it completely.
Onichomycosis is a common infectious disease that ends as soon as its pathogen is removed from the body. This can only be prevented by improper handling or mistakes made by the patient. The peculiarity of onychomycosis is that the fungus is located under the nail plate (in the nail bed). Not all LPs can penetrate so deeply. Therefore, the use of special forms of external agents or systemic antifungal therapy for the treatment of onychomycosis is recommended today. Moreover, treatment should be continued even after all symptoms of the fungal infection have resolved. You can only stop taking medications that show that the fungus is no longer in the tissues after only 3 repeated examinations (microscopy). In addition, the use of antifungal agents should be combined with proper nail and foot care. this reduces the risk of new relapses.
In vain we treat the fungus with external agents.
Modern forms of external formulations allow the creation of high concentrations of the antifungal agent in the affected area. However, external agents are not absorbed into the systemic circulation, have a broader spectrum of action, and have a low risk of developing resistance. Unfortunately, not all external drugs can penetrate the thickness of the nail, especially the nail bed tissue where most of the pathogens are located. Therefore, it is recommended to combine topical therapy with the removal of the nail plate or the use of keratolytic agents - urea or salicylic acid preparations. This is especially important if onychomycosis is associated with nail hyperkeratosis. Generally, monotherapy with external agents is used in cases where 1-2 fingernails or 1/3 of the surface of the nail plates are touched. In other cases, external agents are used in combination with systemic antifungal drugs.
Antifungal tablets are very dangerous and toxic.
Indeed, due to the long duration of antifungal therapy (up to 12 months in some cases), there is a risk of side effects and toxic effects on the liver. But today, methods have been developed that allow you to minimize this danger. Thus, for example, some antifungal drugs are used in a pulse therapy regimen: i. e. short courses of 5-7-10 days with a 21-day break. There are systemic antifungals that can only be taken 1-2 times a week. There are antifungals with a high safety profile that, when administered in therapeutic doses, do not adversely affect liver cells even after prolonged continuous use. Therefore, the most important thing is not to take systemic antifungals without the appointment and supervision of a doctor. Only a dermatologist can prescribe such funds.
If you choose the right medicine, the fungus can heal in a week.
It is only possible to stop the development of a fungal infection in a short time if the infection has occurred recently and the pathogen of onychomycosis has not had time to penetrate deep into the tissues surrounding the nail. But unfortunately, few patients seek medical help at this stage, most often treatment for onychomycosis begins in the later stages when the nail plate (or even more) is severely affected and the process of dystrophy or hyperkeratosis is actively ongoing in the surrounding tissues. In such a situation, no medication will help to solve the fungal problem quickly, even if the treatment is combined with the complete removal of the affected nail plate, because it takes about 3 months to repair the nail. In a relatively short period of time, about 4-6 weeks, you can only reduce the most noticeable symptoms of onychomycosis. But the pathogen of the infection, especially in the form of spores, remains in the tissues. And you can only get rid of this unpleasant disease after completing the treatment prescribed by your doctor.

























